Dr. W. Andy Knight and Dr. Rosalind Warner
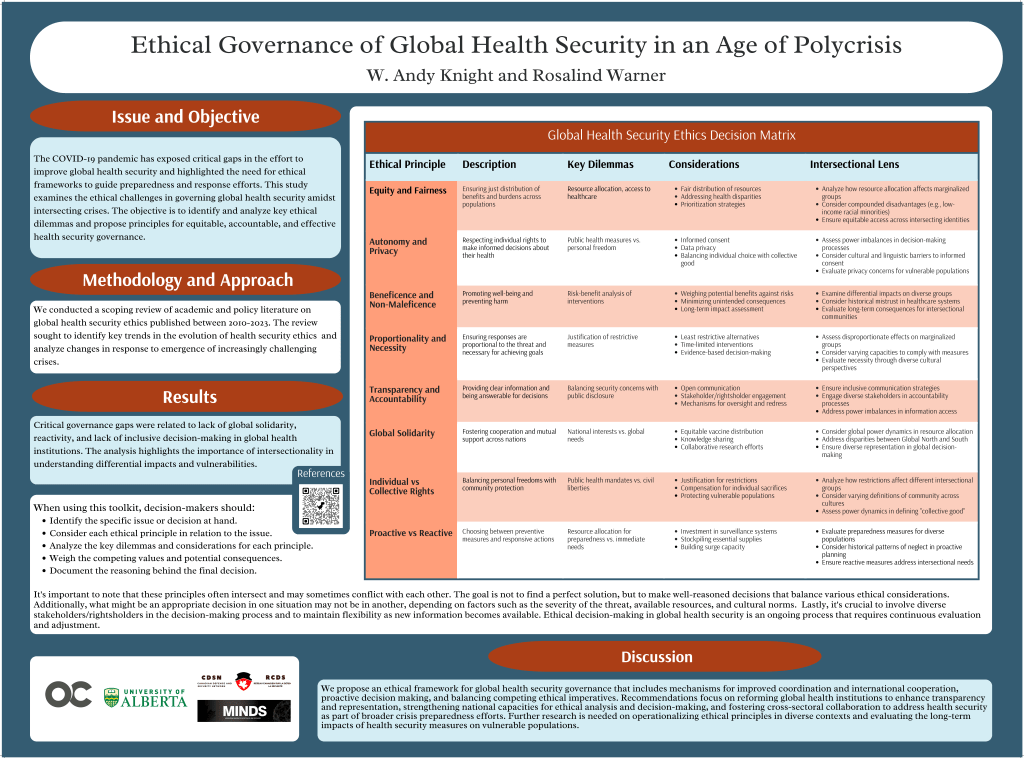
The COVID-19 pandemic has exposed critical gaps in the effort to improve global health security and highlighted the need for ethical frameworks to guide preparedness and response efforts. This study examines the ethical challenges in governing global health security amidst intersecting crises. The objective is to identify and analyze key ethical dilemmas and propose principles for equitable, accountable, and effective global health security governance.
Poster prepared for Canadian Association for Global Health Conference October 23-25, 2024
Vancouver, BC Canada
Selected References
Equity and Fairness
Balabanova, D., McKee, M., Mills, A., Walt, G., & Haines, A. (2010). What can global health institutions do to help strengthen health systems in low income countries. Health Policy Research and Systems, 8, 1–11. https://doi.org/10.1186/1478-4505-8-22
Connolly, K. (n.d.). Freedom and Fairness: Covid Vaccine Passport Plans Cause Global Unease. The Guardian. Guardian News and Media. https://www.theguardian.com/world/2021/feb/07/freedom-and-fairness-covid-vaccine-passport-plans-cause-global-unease.
Deivanayagam, T. A., English, S., Hickel, J., Bonifacio, J., Guinto, R. R., Hill, K. X., Huq, M., Issa, R., Mulindwa, H., Nagginda, H. P., de Morais Sato, P., Selvarajah, S., Sharma, C., & Devakumar, D. (2023). Envisioning environmental equity: Climate change, health, and racial justice. The Lancet, 402(10395), 64–78. https://doi.org/10.1016/S0140-6736(23)00919-4
Dewan, A. (n.d.). A Fight between the EU and UK Reveals the Ugly Truth about Vaccine Nationalism. CNN. Cable News Network. https://www.cnn.com/2021/01/30/europe/uk-eu-astrazeneca-vaccine-nationalism-gbr-intl/index.html.
Elbe, S. (2010). A Global Pharmacy for the poor? Endemics and Other Human Insecurities. In Security and Global Health (p. 220). Polity Press.
Loh, M. (n.d.). Who Chief: It’s ‘Seriously Disappointing’ That Rich Countries Are Ordering Booster Shots While Other Nations Need Vaccines. Insider. Insider. https://www.insider.com/who-admonishes-rich-countries-buying-booster-shots-others-need-vaccines-2021-7.
O’Neill Institute For National & Global Health Law Georgetown Law & Center for Transformational Health Law. (2022, April). Equitable Access Review of CEPI’s COVID-19 Vaccine Development Agreements. https://oneill.law.georgetown.edu/publications/equitable-access-review-of-cepis-covid-19-vaccine-development-agreements/
Smith, R., Beaglehole, R., Woodward, D., Drager, N., & Smith, R. (2003). Global public goods for health: Health economic and public health perspectives. Oxford University Press.
Van De Pas, R., Widdowson, M. A., Ravinetto, R., N Srinivas, P., Ochoa, T. J., Fofana, T. O., & Van Damme, W. (2022). COVID-19 vaccine equity: A health systems and policy perspective. Expert Review of Vaccines, 21(1), 25–36. https://doi.org/10.1080/14760584.2022.2004125
Beneficence and Non-Maleficence
McDougall, L. (2016). Discourse, ideas and power in global health policy networks: Political attention for maternal and child health in the millennium development goal era. Globalization and Health, 12(1), 309. https://doi.org/10.1186/s12992-016-0157-9
Pike, J., Bogich, T., Elwood, S., Finnoff, D. C., & Daszak, P. (2014). Economic optimization of a global strategy to address the pandemic threat. Proceedings of the National Academy of Sciences of the United States of America, 111(52), 18519–18523. https://doi.org/10.1073/PNAS.1412661112
Autonomy and Privacy
Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A., Srouji, S., & Sela, E. (2020). Vaccine hesitancy: The next challenge in the fight against COVID-19. European Journal of Epidemiology, 35(8), 775–779. https://doi.org/10.1007/S10654-020-00671-Y/FIGURES/3
Packard, R. M. (2016). A History of Global Health: Interventions Into the Lives of Other People.
Sallam, M. (2021). Covid-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines, 9(2), 1–15. https://doi.org/10.3390/VACCINES9020160
Salmon, D. A., Haber, M., Gangarosa, E. J., Phillips, L., Smith, N. J., & Chen, R. T. (1999). Health consequences of religious and philosophical exemptions from immunization laws: Individual and societal risk of measles. Journal of the American Medical Association, 282(1), 47–53. https://doi.org/10.1001/jama.282.1.47
Turnbull, S. (n.d.). Here’s What Canada’s Privacy Commissioners Say Must Be Considered for Vaccine Passports. Coronavirus. CTV News. https://www.ctvnews.ca/health/coronavirus/here-s-what-canada-s-privacy-commissioners-say-must-be-considered-for-vaccine-passports-1.5434967?fbclid=IwAR1Qu_olw-hmvgTkxJpDJCIYhCQ2mwKUKoEb1b3BchNJrjX7LU6YFAYdk7A.
Global Solidarity
Acharya, A. (n.d.). A ‘Third Way’ for World Order after Covid-19: Think Global Health. Council on Foreign Relations. https://www.thinkglobalhealth.org/article/third-way-world-order-after-covid-19.
Duff, J. H., Liu, A., Saavedra, J., Batycki, J., Morancy, K., Stocking, B., O Gostin, L., Galea, S., Bertozzi, S., Zuniga, J. M., Alberto-Banatin, C., Dansua, A. S., del Rio, C., Kulzhanov, M., Lee, K., Scaglia, G., Shahpar, C., Ullmann, A. J., Hoffman, S. J., … Szapocznik, J. (2021). A global public health convention for the 21st century. Lancet Public Health, 6(6), 428–433.
Eaton, L., & Humphreys, G. (2020). The need for a coordinated international pandemic response. Bulletin of the World Health Organization, 98(6), 378–379. https://doi.org/10.2471/BLT.20.020620
Gostin, L. O., & Friedman, E. A. (2014). Ebola: A crisis in global health leadership. The Lancet, 384(9951), 1323. https://doi.org/10.1016/s0140-6736(14)61791-8
Gupta, N., Singh, B., Kaur, J., Singh, S., & Chattu, V. K. (2021). Covid-19 pandemic and reimagination of multilateralism through global health diplomacy. Sustainability (Switzerland), 13(20). https://doi.org/10.3390/SU132011551
Heymann, D. (2006). SARS and emerging infectious diseases: A challenge to place global solidarity above national sovereignty. Annals Academy Of Medicine Singapore, 35(5), 350.
Jamison, D. T., Summers, L. H., Alleyne, G., Arrow, K. J., Berkley, S., Binagwaho, A., Bustreo, F., Evans, D., Feachem, R. G. A., Frenk, J., Ghosh, G., Goldie, S. J., Guo, Y., Gupta, S., Horton, R., Kruk, M. E., Mahmoud, A., Mohohlo, L. K., Ncube, M., … Yamey, G. (2015). Global health 2035: A world converging within a generation. The Lancet, 382(9908), 1898–1955. https://doi.org/10.1016/s0140-6736(13)62105-4
Taghizade, S., Chattu, V. K., Jaafaripooyan, E., & Kevany, S. (2021). COVID-19 Pandemic as an Excellent Opportunity for Global Health Diplomacy. Frontiers in Public Health, 9. https://doi.org/10.3389/FPUBH.2021.655021
Tong, S., Samet, J. M., Steffen, W., Kinney, P. L., & Frumkin, H. (2023). Solidarity for the Anthropocene. Environmental Research, 235, 116716. https://doi.org/10.1016/j.envres.2023.116716
Individual vs Collective Rights
Global Health Governance: Health Security Vs. Human Rights? (n.d.). Australian Institute of International Affairs. Retrieved 23 September 2023, from https://www.internationalaffairs.org.au/australianoutlook/global-health-governance-health-security-vs-human-rights/
HAYDEN, P. (2012). The human right to health and the struggle for recognition. Review of International Studies, 38(3), 569–588. https://doi.org/10.1017/S0260210511000556
Hollingsworth, T. D., Ferguson, N. M., & Anderson, R. M. (2007). Frequent travelers and rate of spread of epidemics. Emerging Infectious Diseases, 13(9), 1288–1294. https://doi.org/10.3201/EID1309.070081
Hostmaelingen, N., & Bentzen, H. B. (2020). How to operationalise human rights for COVID-19 measures. BMJ Global Health, 5(7), 1–4. https://doi.org/10.1136/bmjgh-2020-003048
Kata, A. (2012). Anti-vaccine activists, Web 2.0, and the postmodern paradigm—An overview of tactics and tropes used online by the anti-vaccination movement. Vaccine, 30(25), 3778–3789. https://doi.org/10.1016/J.VACCINE.2011.11.112
UNGA (United Nations General Assembly). (2022, July 28). UN General Assembly declares access to clean and healthy environment a universal human right | UN News. https://news.un.org/en/story/2022/07/1123482
Proactive vs Reactive
Ayala, A., Brush, A., Chai, S., Fernandez, J., Ginsbach, K., Gottschalk, K., Halabi, S., Hosangadi, D., Mapatano, D., Monahan, J., Moretti, C., Pillinger, M., Ramirez, G. S., & Rosenfeld, E. (2022). Advancing Legal Preparedness through the Global Health Security Agenda. Journal of Law, Medicine & Ethics, 50(1), 200–203. https://doi.org/10.1017/JME.2022.26
Cáceres, S. B. (n.d.). Global Health Security in an Era of Global Health Threats—Volume 17, Number 10—October 2011—Emerging Infectious Diseases journal—CDC. https://doi.org/10.3201/eid1710.101656
de Guttry, A. (2020). Is the International Community Ready for the Next Pandemic Wave? A Legal Analysis of the Preparedness Rules Codified in Universal Instruments and of their Impact in the Light of the COVID-19 Experience. Global Jurist, 20(3), 1–41.
Fukuda-Parr, S. (2022). When indicators fail: SPAR, the invisible measure of pandemic preparedness. Policy and Society. https://doi.org/10.1093/polsoc/puac024
Gostin, L. O., & Ayala, A. S. (2017). Global Health Security in an Era of Explosive Pandemic Potential. Journal of National Security Law & Policy, 9, 53.
Knight, W. A., & Reddy, K. S. (2020). Caribbean response to COVID-19: A regional approach to pandemic preparedness and resilience. The Round Table, 109(4), 464–465. https://doi.org/10.1080/00358533.2020.1790759
Lal, A., Abdalla, S. M., Chattu, V. K., Erondu, N. A., Lee, T., Singh, S., Abou-taleb, H., Morales, J. V., & Phelan, A. (2022). Health Policy Pandemic preparedness and response: Exploring the role of universal health coverage within the global health security architecture. 22, 1–9.
Manika, S. (2021). Fostering preparedness for COVID-19 in cities: How cities can support the healthcare system by efficiently managing emergency funding. TPR: Town Planning Review, 92(3), 293–299.
Nelson, C., Lurie, N., Wasserman, J., & Zakowski, S. (2007). Conceptualizing and Defining Public Health Emergency Preparedness. American Journal of Public Health, 97, S9–S11. https://doi.org/10.2105/ajph.2007.114496
The Petrie-Flom Center Staff. (2022, October 24). Using Legal Preparedness to Minimize Liability Barriers to Accessing Pandemic Vaccine and Medical Countermeasures. Bill of Health. https://blog.petrieflom.law.harvard.edu/2022/10/24/using-legal-preparedness-to-minimize-liability-barriers-to-accessing-pandemic-vaccine-and-medical-countermeasures/
Virtual Blockbuster Bird Flu and the Pandemic of Preparedness Planning. (2018). In Stefan Elbe, Pandemics, Pills, and Politics: Governing Global Health Security (p. 106). Johns Hopkins University Press
Proportionality and Necessity
Dace, H., Miller, B., Ramli, R., Sleat, D., Thorne, E., & Wain, R. (n.d.). The New Necessary: How We Future-Proof for the Next Pandemic. Tony Blair Institute for Global Change. Retrieved 8 July 2021, from https://institute.global/policy/new-necessary-how-
Dzau, V. J., & Rodin, J. (2015). Creating a global health risk framework. New England Journal of Medicine, 373(11), 991–993. https://doi.org/10.1056/nejmp1509136
Knight, W. A., & Oriola, T. B. (2022). Vaccine nationalism, violent extremist problematique and state management of combat-related deaths. Https://Doi.Org/10.1080/19392206.2022.2059923, 15(1), 1–3. https://doi.org/10.1080/19392206.2022.2059923
Lal, A., Abdalla, S. M., Chattu, V. K., Erondu, N. A., Lee, T., Singh, S., Abou-taleb, H., Morales, J. V., & Phelan, A. (2022). Health Policy Pandemic preparedness and response: Exploring the role of universal health coverage within the global health security architecture. 22, 1–9.
Samaan, G., Patel, M., Spencer, J., & Roberts, L. (2004). Border screening for SARS in Australia: What has been learnt? Medical Journal of Australia, 180(5), 220–224. https://doi.org/10.5694/J.1326-5377.2004.TB05889.X
The Lancet: New report details “massive global failures” of COVID-19 response, calls for improved multilateral cooperation to end pandemic and effectively manage future global health threats. (2022). SDSN Newsletter. https://www.unsdsn.org/the-lancet-new-report-details-massive-global-failures-of-covid-19response-calls-for-improved-multilateral-cooperation-to-end-pandemic-andeffectively-manage-future-global-health-threats
Transparency and Accountability
Lindmeier, C. (2021). WHO, Germany launch new global hub for pandemic and epidemic intelligence. World Health Organization. https://www.who.int/news/item/05-05-2021-who-germany-launch-new-global-hub-for-pandemic-and-epidemic-intelligence
MacIntyre, C. R., & Aginam, O. (2022, June 22). At what point is a disease deemed to be a global threat? Here’s the answer. The Conversation. http://theconversation.com/at-what-point-is-a-disease-deemed-to-be-a-global-threat-heres-the-answer-185547
Ozawa, S., Paina, L., & Qiu, M. (2016). Exploring pathways for building trust in vaccination and strengthening health system resilience. BMC Health Services Research, 16, 131–141. https://doi.org/10.1186/S12913-016-1867-7
Sturmberg, J. P. (2020). Approaching complexity—Start with awareness. Journal of Evaluation in Clinical Practice, 26(3), 1030–1033. https://doi.org/10.1111/JEP.13355






You must be logged in to post a comment.